How to Treat Plantar Fasciitis: Early, Developing, and Chronic Stages Explained
By MADI-BONE CLINIC | Gangnam (Seolleung Station)
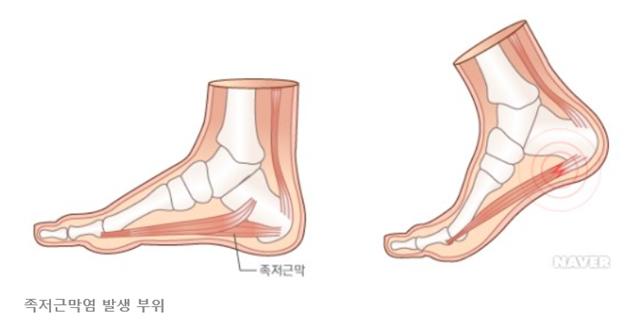
Plantar Fasciitis Needs Different Treatment at Each Stage
Plantar fasciitis does not behave the same in the first week as it does in the third month.
Many patients stay stuck in pain because they use a single method for a condition that evolves through phases.
This guide explains how we treat plantar fasciitis from early → developing → chronic stages using an evidence-based, structured approach.
Stage 1 — Early Phase (Day 1 to ~2 Weeks)
Goal: Calm the irritated plantar fascia
In the early inflammatory and reactive phase, the fascia is overloaded and highly sensitive. The focus is on reducing mechanical stress.
1) Activity Modification
- Reduce walking volume, running, hiking, and prolonged standing.
- Avoid barefoot walking on hard floors.
2) Footwear Adjustments
- Use cushioned athletic shoes.
- Avoid flat, thin-soled shoes.
- Flip-flops and minimalist shoes are not ideal at this stage.
3) Gentle Stretching (No Aggressive Pulling)
- Light calf stretch: 20–30 seconds, 2–3 reps.
- Gentle plantar fascia stretch in sitting.
Early stretching of the plantar fascia has been shown to improve pain and function.
Radford et al., RCT
4) Ice for Pain Relief
- Roll a frozen water bottle under the foot for 10–15 minutes.
5) Medication (Optional)
A short course of NSAIDs can help with early-phase symptoms, but they should not be relied on as a long-term solution.
Stage 2 — Developing/Subacute Phase (2 Weeks to ~8 Weeks)
Goal: Restore flexibility and begin strengthening
If pain persists beyond ~2 weeks, the fascia is no longer purely inflamed — it is adapting structurally.
This is where most patients need consistent rehab to prevent chronic progression.
1) Complete Stretching Routine
- Calf stretching (knee straight + knee bent).
- Plantar fascia stretching: 20–30 seconds × 3 reps, twice daily.
- Toe curls and towel scrunch exercises.
2) Strengthening for the Foot Intrinsics
- Short-foot exercise.
- Marble pick-ups.
3) Manual Therapy
Manual soft-tissue treatment of the calf and plantar fascia can reduce tension and improve mobility.
4) Taping (Optional)
Low-dye taping or kinesiology taping can temporarily support the arch and offload the fascia.
5) Orthoses (Case-by-case)
If you have flat feet or very high arches, temporary insoles can help redistribute pressure.
Foot orthoses have demonstrated pain relief benefits for plantar fasciitis in multiple trials and systematic reviews.
Orthoses meta-analysis
Stage 3 — Chronic Phase (8 Weeks and Beyond)
Goal: Stimulate healing, rebuild tissue capacity, and break the cycle
If symptoms last more than two months, plantar fasciitis enters a degenerative phase (like a tendinopathy).
At this point, the fascia needs stimulation and strengthening, not just rest.
1) Structured Strengthening Program
Chronic cases require progressive exercises:
- Calf strengthening (eccentric loading).
- Heavy–slow resistance for calf/foot muscles.
- Progressive plantar fascia loading (within tolerable pain range).
2) Extracorporeal Shockwave Therapy (ESWT)
Shockwave is one of the most effective non-invasive options for chronic plantar fasciitis.
It helps by:
- reducing pain
- stimulating new blood vessel formation
- enhancing tissue regeneration
Shockwave therapy has strong evidence for chronic plantar fasciitis, including RCTs and systematic reviews.
Gerdesmeyer et al., RCT;
Systematic Review
3) Night Splints
For patients with severe morning pain, night splints can help maintain the fascia in a lengthened position during sleep.
4) Injection Options (Selective Use)
We are conservative with injections for plantar fasciitis, but in some cases:
- ultrasound-guided steroid injection for acute severe flares
- PDRN or regenerative injections in chronic cases
Early vs Chronic: Why Timing Matters
Plantar fasciitis is far easier to treat in the first 2–4 weeks.
Once it becomes chronic, treatment requires:
- more structured strengthening
- longer rehabilitation
- biological stimulation (ESWT or regenerative approaches)
The key is recognizing symptoms early and acting before the fascia becomes degenerative.
When to Visit a Clinic
- Pain lasts longer than 2–3 weeks
- Pain is severe in the morning or after rest
- Walking or standing becomes difficult
- Symptoms keep returning despite rest
- You have flat feet, high arches, or other foot structure concerns
MADI-BONE CLINIC (Seolleung Station, ~3 min on foot)
MADI-BONE CLINIC
3F, 428 Seolleung-ro, Gangnam-gu, Seoul
Seolleung Station (Line 2), Exit 1 — ~3 minutes on foot
02-736-2626
⏰ Mon–Fri 09:30–18:30 / Sat 09:30–13:00 (Closed Sundays & Public Holidays)
References
- Radford JA, et al. Effectiveness of calf and plantar fascia stretching for plantar heel pain. BMJ. PubMed
- Whittaker GA, et al. Foot orthoses for plantar heel pain: systematic review & meta-analysis. PubMed
- Gerdesmeyer L, et al. Shockwave therapy for chronic plantar fasciitis: RCT. PubMed
- Thomson CE, et al. ESWT systematic review for plantar heel pain. PubMed
This article is for educational purposes and does not replace an individual medical evaluation or treatment plan.