Learn when MRI is essential—especially when X-rays are normal—and which hidden injuries require advanced imaging.
When MRI Truly Matters for Injury Detection
By MADI-BONE CLINIC — Gangnam (Seolleung Station)
“My X-ray Was Normal — So Why Do I Still Hurt?”
In orthopedic practice, this question appears daily.
X-rays often reveal fractures clearly,
yet many patients continue experiencing significant pain even when imaging looks normal.
This is when MRI becomes invaluable.
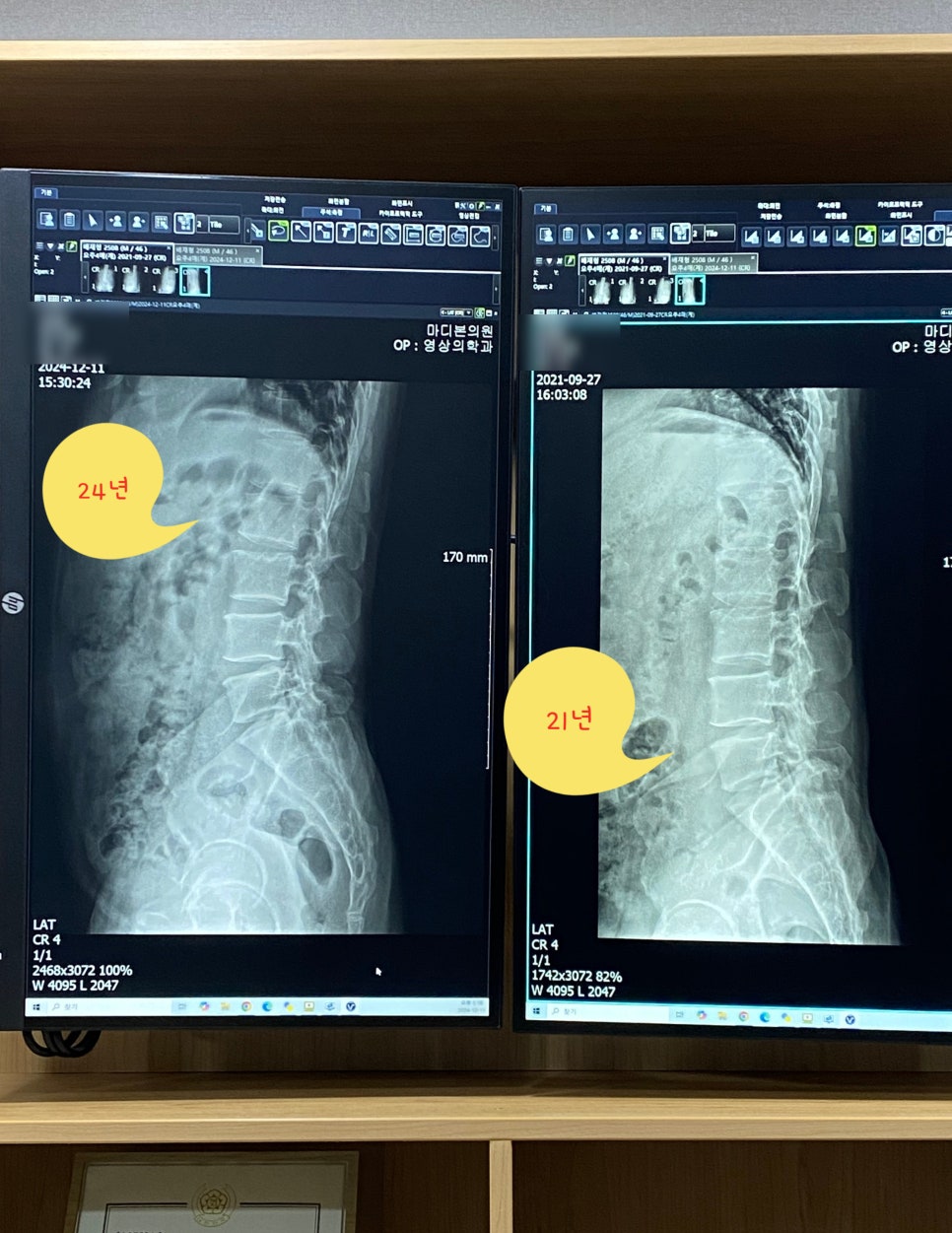
What X-ray Can—and Cannot—See
X-ray is excellent for:
- fractures
- joint alignment
- bone degeneration
But it cannot visualize:
- ligaments
- tendons
- cartilage
- nerve irritation
- bone marrow injury
This is why someone may be told:
“Your X-ray is fine — but the pain remains.”
When MRI Is Truly Needed
At MADI-BONE CLINIC, MRI is recommended when:
- pain persists beyond 2–4 weeks
- swelling or weakness does not improve
- functional movements remain restricted
- instability is suspected
MRI visualizes soft tissue architecture, marrow reaction and hidden injury patterns.

Hidden Injuries That MRI Detects
1. TFCC Tears
X-rays often miss triangular fibrocartilage complex (TFCC) damage.
MRI detects inflammatory reaction, tearing or degeneration.
2. Ligament Sprains and Partial Ruptures
Common in ankle, wrist, elbow and knee injuries — especially after falls.
3. Tendon Degeneration and Tear
Rotator cuff, Achilles and elbow tendons often look “normal” on X-ray but may show structural breakdown on MRI.
4. Cartilage and Meniscus Injury
Painful, yet invisible on standard radiographs.
5. Bone Marrow Edema — The Unknown Pain Generator
Bone bruising or marrow swelling causes intense pain despite normal radiographs.
MRI shows this clearly.
MRI is essential for detecting occult soft tissue and marrow injury.
MRI Detection Study
Why MRI Reveals So Much More Than X-ray
While X-ray visualizes skeleton structure,
MRI evaluates:
- fluid and inflammation
- tissue tearing
- degeneration
- nerve involvement
This makes it indispensable for persistent pain with unclear cause.
Common Scenarios Where MRI Changes Treatment
1. Someone Fell and “Sprained” Their Wrist
MRI may reveal TFCC injury or occult bone bruising.
2. Chronic Knee Pain With Normal X-ray
MRI often discovers meniscal tear or cartilage damage.
3. Resolving but Relapsing Ankle Pain
MRI identifies ligament instability or cartilage defect.
MRI Is Not Always Needed — But It Matters at the Right Time
Not every patient needs MRI immediately — but when symptoms persist or functional limitation exists,
MRI identifies conditions X-ray cannot.
Internal Links — Related Insights
- Why Pain Persists Without Fracture
- Winter Falls: What Hurts Most and Why
- Why TFCC Injuries Rise in Winter
Frequently Asked Questions (FAQ)
1. Should MRI be first-line testing?
Not usually — most musculoskeletal evaluation starts with X-ray because it excludes fractures and is cost-effective.
MRI is used when deeper structures require visualization.
2. Why did my pain start weeks after injury?
Soft-tissue or marrow-related injury can become more symptomatic once surrounding swelling resolves.
3. Is MRI necessary for every case?
No — but in persistent pain cases, MRI changes treatment decisions significantly.
MADI-BONE CLINIC — Seolleung Station
MADI-BONE CLINIC
3F, 428 Seolleung-ro, Gangnam-gu, Seoul
Seolleung Station Exit 1 — 3 minutes on foot
02-736-2626
⏰ Mon–Fri 09:30–18:30 / Sat 09:30–13:00